What is tubal sterilisation (ligation and sometimes referred to as permanent contraception)?
When a woman no longer wants to have children (for example the family is complete, or when other traditional contraceptive methods (such as the pill or an IUD) are no longer appropriate or recommended, then a woman can legally (Loi de juillet 2001) opt for tubal sterilization or as it is more commonly termed “getting your tubes tied”.
During tubal ligation surgery, both fallopian tubes are blocked. This procedure prevents the egg and male sperm from fusing and prevents pregnancy from occurring.
Tubal ligation surgery used to be performed via access through the abdomen. Nowadays with surgical advances and specifically with coelioscopic procedures being available, the surgeon can now clip each of the fallopian tubes using a thin endoscopy. This method uses a small incision to insert the endoscope through the belly button. The fallopian tubes are clipped with special endoscopic clips or tied off with special elastics. This surgery is carried out under general anesthesia. The procedure is permanent. The clips can only be removed or the elastics untied via another round of surgery. Once the clips are undone the tubes require repair using microsurgery and regaining fertility is not guaranteed.
Today, thanks to advances in hysteroscopy procedures, the clinician can now view the start of the fallopian tubes (specifically, the proximal tubal opening). The surgeon can then insert a fallopian tube occlusion device. This is usually without anesthesia as it is almost painless (there are no incisions or scars).
The occlusion device progressively blocks the tubes and prevents the egg and male sperm from fusing and prevents pregnancy. This contraceptive method is irreversible.
French law requires that a woman takes 4 months to consider the consequences of this contraceptive procedure before proceeding. This period of reflection should be professionally accompanied in a public or private hospital even if the actual contraception procedure takes place elsewhere. The procedure can take place on an outpatient basis in a medically equipped facility and the patient can return home quickly within a matter of minutes or a few hours after the procedure is completed.
During this process patients will have been given all information available on traditional contraception methods and will have stated their express wish to proceed with permanent irreversible contraception.
What is ESSURE® ?
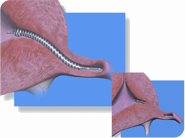
 ESSURE® is a fallopian tube occlusion device. It is a small insert that the doctor positions into the first segment of your fallopian tubes through the natural pathways. The inserts conform to the shape of the tube and over 3 months (approximately) progressively form a complete barrier preventing sperm from reaching the egg (gametes cannot fuse).
ESSURE® is a fallopian tube occlusion device. It is a small insert that the doctor positions into the first segment of your fallopian tubes through the natural pathways. The inserts conform to the shape of the tube and over 3 months (approximately) progressively form a complete barrier preventing sperm from reaching the egg (gametes cannot fuse).
 Using the hysteroscopy procedure, the gynecologist positions soft and flexible micro-implants (micro-inserts) via the body’s natural pathways (navigating through the vagina and cervix and up to the uterus) in the first segment of the fallopian tubes.
Using the hysteroscopy procedure, the gynecologist positions soft and flexible micro-implants (micro-inserts) via the body’s natural pathways (navigating through the vagina and cervix and up to the uterus) in the first segment of the fallopian tubes.
These inserts are a type of stent made from a stainless steel alloy (with Nitinol™, a metal alloy of nickel and titanium, which raises the question whether women with nickel allergies would suffer adverse reactions) and the centre of the stent contains Polyethylene terephthalate (PET). PET provokes an inflammation response which produces fibrosis and blocks the fallopian tube. The ESSURE® method can be carried out in a clinic or a hospital usually on an outpatient basis and without general anesthesia. No incisions are needed and so there is no scarring. Most women can expect to go home on the day of the Essure® procedure and return to normal activities the same day or in the days immediately following the procedure.
During the first 3 months following the Essure® procedure, the body progressively produces fibrous tissue around the implant which totally blocks the fallopian tubes. Women must use another form of birth control until the 3 months are up as it takes this time for the tubes to be completely blocked.
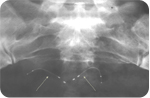
Three months after the Essure® procedure, the gynecologist performs an Essure Confirmation Test to confirm the correct position of the implants and that the tubes are completely blocked thus indicating permanent contraception. The Confirmation Test is carried out via an x-ray of the abdomen or an ultrasound scan of the uterus. The implants can be viewed and assessed as to their position and whether or not the tubes are completely blocked. When the test confirms that the implants are well positioned and the tubes are blocked then test results show that the woman has zero chance of falling pregnant.
The implants do not interfere with a woman’s menstrual cycle or her hormones so women should not notice anything different with their normal menstrual rhythm. This form of contraception is permanent and irreversible. The implants can only be removed by surgery and fertility is not restored.
How does the Essure® procedure work?
Once the decision to opt for Essure® has been taken during the consultation period, and the consent form has been signed, and the 4 month period for reflection has passed, then the procedure can be scheduled. The patient meets the anaesthetist in a public or private hospital at least 48 hours before the procedure. (Essure® is covered by the French Social Security subsidisation system.)
- The operative hysteroscopy procedure is carried out on the operating table. In general no anesthesia is administered (should some patients be particularly sensitive or experience discomfort during the procedure, then the anaesthetist can give analgesia (this is why the patient meets the anaesthetist at least 48 hours beforehand). Most often analgesia is given in the form of an anti-inflammatory suppository one hour before the procedure. This reduces uterine contractions and so facilitates the mechanics of the procedure.
- A hysteroscope is delicately inserted into the uterus and the proximal tubal opening is sighted. The micro-implants (Essure®) are loaded into the hysteroscope and placed (they are slid into the tubes and then put into position) into each fallopian tube.
- This is painless and lasts between 5 and 10 minutes.
- In a minority of cases (5%) it is not possible to place the implants correctly into position. This is the main disadvantage of this method. It occurs only in rare cases and has been discussed in published medical studies.
- After between 30 minutes and a few hours (if analgesia has been used) the patient can return home or return to normal working activities. Some very light bleeding/spotting may occur and some temporary cramping may also occur,
- During the following 3 months the patient should not experience any pain nor bleeding related to the implants.
- One month after the procedure, the gynecologist schedules a check-up and will usually perform an ultrasound scan of the pelvic area to verify that the implants are in the correct position.
- Three months after the procedure, the gynecologist performs a confirmation test. The abdomen is x-rayed and an ultrasound scan is normally retaken. When the confirmation test is positive then there is no need to continue taking other forms of birth control as this sterilization procedure is deemed successful. Failure rates are 0.05% after one year and 0.02% after 4 years. Up to now at our centre, no patient has fallen pregnant after a successful Essure® procedure.