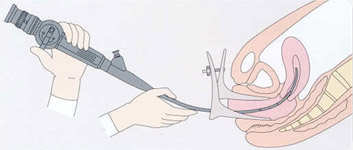
This is the inspection of the cervix and the uterine cavity using a very small endoscope that is inserted into the uterus.
Hysteroscopy procedures are performed between the 5th and the 14th day of the menstrual cycle*. This is to:
- better view the uterine area (because the patient’s period is finished)
- ensure the absence of pregnancy (because this time period occurs before ovulation)
*This does not apply to women experiencing the menopause or receiving treatment to block their menstrual cycle.
When the endoscope that is used is very thin, and when the method for distending the uterine cavity is “gentle” (using low pressure saline solution), then diagnostic hysteroscopy procedures are relatively painless (mean scoring just 2/10 on a pain scale).
No special medical preparation or medication is required before a diagnostic hysteroscopy can be performed.
Pain is rarely experienced after a diagnostic hysteroscopy but the patient may experience some light bleeding for a few hours after the procedure.
As a matter of course, endoscopes and all the instruments used are carefully disinfected so as to avoid the risk of nosocomial infection.
When are diagnostic hysteroscopy procedures performed?
Diagnostic hysteroscopy is a visual examination of the uterine cavity that is used for these situations:
- Infertility or sterility; in order to verify that nothing could impede the implantation of an embryo,
- Assisted Reproductive Technology (ART) programs (including IVF, insemination, egg donation); in order to check the absence of any lesions that may interfere with embryo implantation (impediments such as an infection or an inflammation of the mucous membrane (endometrium) are only visible with a diagnostic hysteroscopy),
- Abnormal pelvic ultrasound scan results; so that the clinician can visually examine the area the ultrasound picked up as abnormal and decide as to the necessity of any surgical treatment,
- Abnormal uterine bleeding (AUB) (including metrorrhagia (bleeding between cycles) and menorrhagia (prolonged or huge bleeding); in order to determine if any polyps, fibroma, or endometrial abnormalities (abnormalities in the lining of the uterus) exist,
- Postmenopausal bleeding; in order to rule out any cancer or precancerous lesions,
- Abnormal hysterosalpingography (HSG) results; so that any uterine cavity abnormalities can be examined,
- Uterine adhesions; so that any adhesions can be inspected and assessed as to their impact on fertility,
- Uterine malformation; so that any impact on fertility can be assessed (for example in the case where the cranial part of the uterus remains bifurcated resulting in a uterus with two horns),
- Intrauterine device (IUD) displacement or difficulty with IUD string location; so that the clinician can reposition the IUD and or retrieve the string and if necessary remove the IUD (IUD removal does not require general anesthesia),
- Uterine polyps; in order to examine their type and position,
- Post uterine surgical monitoring; in order to check that the healing process is well underway and that the uterine cavity is healthy,
- Recurrent pregnancy loss (RPL); in order to check if there are any intrauterine reasons (for example fibroma) for repeated miscarriages, or if the uterus has been compromised after a miscarriage (for example uterine adhesions or retained placental fragments), which may impact future embryo implantation


