What is a uterine septum?
The uterus is a hollow organ (a type of muscular pocket) which enables an embryo to be implanted. Within the uterus the embryo can develop into a foetus and after 9 months gestation a baby is ready for birth. Although the uterus is a hollow organ it is the result of the fusion of two hollow tubes called the Müllerian ducts. During the development of the embryo, the ducts attach to each other to form a uterus. The top of the uterus ends with two tubes (corresponding to the Fallopian tubes) and two ovaries (evidence today of the embryos symmetrical development).
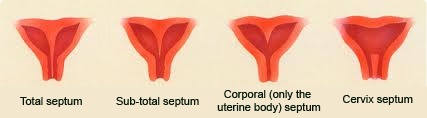
In some cases the ducts fail to attach correctly. Abnormalities of varying significance result. These can be the development of two uterine cavities, with each uterus even having its cervix and vagina! Less significant abnormalities include the maintenance of a wall or partition (that should have normally disappeared) which splits the uterus into two compartments.
What are the consequences of a uterine septum?
This is a difficult question to answer given that probably most uterine septa go unnoticed insofar as they do not impact the female reproductive system.
Ultrasound scans or hysteroscopy procedures performed for various reasons or as part of fertility assessment can diagnose the presence of uterine septua.
Uterine septa can increase the likelihood of miscarriage, premature births, abnormal delivery positions (such as breech or transverse presentation). Nevertheless, it is quite likely that most pregnancies in women with uterine septum progress normally with =out any adverse consequences.
This is why treatment of uterine septa is not systematic but rather case by case depending on the individual’s clinical history.
How are uterine septa diagnosed?
Ultrasound scans (best performed via the vagina) enable the clinical to sight any septum and examine it height, thickness and blood supply.
Most importantly, the scan enables the clinician to determine if:
the uterus has an internal partition or
there are two uterine cavities (the Müllerian ducts failed to fuse), in which case an operative hysteroscopy is not the recommended treatment. In situations of doubt an MRI (magnetic resonance imagery) scan can sometimes allow a better view of the inside of the uterus.
How are uterine septa treated?
Operative hysteroscopy procedures have revolutionised uterine septum treatment. Twenty years ago (in the 1990s) treatment required opening the abdominal wall and then the uterus in order to cut through the partition and restore a normal sized uterine cavity. This treatment was quite significant and rendered the uterus fragile given that it had to be surgically opened.
With advances in endoscope development and especially in operative hysteroscopy procedures today’s treatment involves sliding inside the uterus and carefully dividing the septum so as to restore a single uterine cavity.
This is a delicate treatment: excessive dividing of the septum may cause a weakening of the uterus during any subsequent pregnancy. Patients may fall pregnant 3-6 months after this procedure and give birth naturally.


